Are you worried about your risk of a heart attack? In today’s world, heart disease accounts for up to 50% of all American deaths. Shockingly, approximately 50% of heart attack sufferers do not survive the event. But fear not, there are tests available that can assess your risk of cardiovascular disease. Unfortunately, most conventional medical systems do not routinely perform these tests. Typically, doctors limit cardiovascular examinations to simpler tests, such as measuring total cholesterol.
The Patient and the Problems
Let me share the real-life story of one of my patients, giving you an insight into how we assessed his chronic issues and gained a better understanding of his cardiovascular health. Hopefully, this will inspire you to take charge of your own well-being and work towards a state of optimal health.
Our patient, a 50-year-old male, was plagued by chronic pain throughout his body, particularly in his lower back.
The Comprehensive Lab Analysis
I always conduct a thorough evaluation using a total of six tests. Below, I’ll provide a list of these tests along with their corresponding costs, which I typically incur. These tests include:
In addition, there is a $10 draw fee, resulting in a total cost of $120. By investing just $120, we can gain a clear understanding of your cardiovascular health and develop an effective plan for your overall well-being.
In the case of the patient we’re discussing, these tests played a crucial role in saving his life.
The Endothelium: The Key to Cardiovascular Health
When we talk about cardiovascular health, we focus on a specific part of the artery called the endothelium. This innermost layer lines all your blood vessels, from arteries to capillaries, and is incredibly thin—only one cell thick.
Despite its delicate nature, the endothelium covers an extensive surface area of up to 14,000 square feet within your body. It acts as an independent organ, producing essential hormones. If the endothelium becomes compromised, it can lead to cardiovascular diseases.
Inflammation plays a vital role in these tests, affecting various systems throughout your body, including the endothelium. Due to its thinness, the endothelium is particularly vulnerable to damage caused by inflammation.
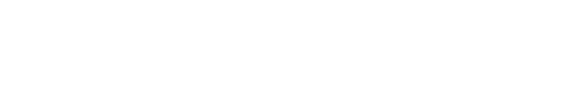
The first test we performed assessed C-reactive Protein (CRP), which serves as a global inflammatory marker. While it cannot pinpoint the exact location of inflammation, it provides an indication of its presence and severity.
Elevated CRP levels in the blood may also indicate the risk of blood clots and other cardiac diseases. Multiple studies have revealed a strong correlation between CRP levels and sudden death.
Ideally, the CRP result should fall within the range of 0 to 3.0, with a value above 3 indicating a heightened risk of heart disease. Personally, I prefer to see this number below 1. In our patient’s case, the test showed a reading of 8.54.
Homocysteine: Another Marker of Inflammation
Homocysteine is another marker I often evaluate to assess inflammation. Research has linked increased homocysteine levels to a higher risk of heart disease, Alzheimer’s, and more. Fortunately, dietary adjustments can often help regulate homocysteine levels.
Typically, the range for homocysteine falls between 0 and 14.5, but I prefer to see it between 5 and 6. In our patient’s case, the result came in at 13.2.
Fortunately, our patient’s hemoglobin A1c readings were not far off from the ideal range, which was good news. The typical range for hemoglobin A1c is 4.8 to 5.6, and I aim to see my patients fall between 5 and 5.2. Our patient’s result was 5.4, slightly higher but within an acceptable range.
Similarly, his fasting insulin showed a slight elevation. The standard range for fasting insulin tests is 2.6 to 24.9, and I prefer my patients to fall between 5 and 6. Our patient’s result was 7.2.
While both of these tests showed only slight elevations, they signify the presence of inflammation that requires timely attention.
Assessing magnesium levels is crucial when evaluating the risk of heart disease. Magnesium is involved in 400 different enzymatic reactions throughout the body. Insufficient magnesium levels hinder the proper functioning of these reactions.
Magnesium also helps relax your arteries. Low levels of magnesium can cause constriction in the muscle wall of your arteries, leading to increased blood pressure and putting additional strain on the endothelium.
Typically, magnesium levels should range from approximately 4 to 7 in most tests. Personally, I prefer to see levels above 6. As of writing this article, we are awaiting the patient’s magnesium test results. However, considering that a significant portion of the US population is magnesium deficient, it is likely that this patient will show low levels.
Understanding LDL and LDL Particle Number
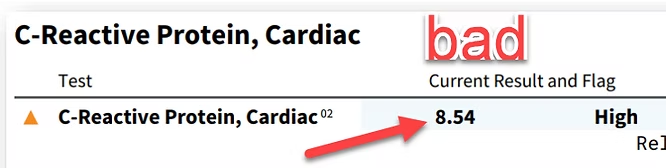
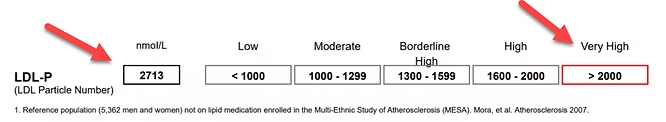
While low-density lipoprotein (LDL) is an essential marker to assess, it can be confusing to interpret. The quantity of LDL in your system is not as critical as the size of the LDL particles.
For instance, two individuals may both have a lab reading of 130mg/dL of LDL. However, one person may have more particles of smaller size, while the other has fewer particles that are larger. The individual with smaller particles faces a significantly higher risk of developing heart disease over time than the one with larger particles.
To illustrate the difference between these particle sizes, imagine fluffy cotton balls gently floating versus small, hard BBs. The cotton balls float harmlessly, while the BBs can lodge between endothelial cells, causing damage.
LDL and HDL Readings
LDL readings come with additional information, including cholesterol levels. Cholesterol itself is not inherently bad. However, like LDL, it needs to be in the appropriate form and quantity. Ideally, I prefer to see triglyceride levels below 100 (our patient measured at 184: high triglycerides means too many carbs) and high-density lipoprotein cholesterol (HDL-C), often referred to as the “good” cholesterol, levels above 40 (our patient measured at 34). Additionally, our patient had low total particle counts of HDL.
Regarding LDL, our patient had a reading of 177, which is relatively high. Moreover, his LDL particle number count (LDL-P) measured at 2,713, an extremely high value. Most particle counts should be lower than 1,000, with anything exceeding 2,000 considered “very high.”
The test I use also measures the size of LDL particles. Ideally, these particles should be larger than 20.6nm, at the very least. Unfortunately, our patient’s readings showed particles sized at 20nm, indicating they were on the smaller side.
Why In-Depth Testing Matters
Focusing solely on one particular test may not provide a comprehensive understanding of a patient’s risk for heart disease. It may only indicate certain symptoms while overlooking the presence of comorbidities that contribute to various problems, increasing the risk of heart issues in the future.
Cholesterol levels often receive excessive attention. However, it is worth noting that 50% of heart attack survivors have normal cholesterol levels. The problem does not lie solely in cholesterol, and relying solely on this marker is inherently flawed.
This is precisely why comprehensive testing is vital. By gathering a wide range of data, we gain a clearer picture of the underlying causes of the problem. This data drives our solutions to your health issues. Most of these readings can be improved through simple lifestyle changes, such as adjustments in diet, exercise, or the use of supplements.
If you are concerned about your heart health, I encourage you to reach out to me. Together, we can conduct tests for all these markers, providing a clear understanding of your current health status and determining the necessary steps to set you on the path to wellness.
Frequently Asked Questions (FAQ)
A comprehensive assessment should include an NMR Lipoprotein Profile (to check LDL particle number and size), High-sensitivity C-Reactive Protein (hs-CRP) to measure inflammation, Homocysteine (another inflammation marker), Hemoglobin A1c and Fasting Insulin for blood sugar control, and Magnesium levels. These tests provide a much clearer picture of cardiovascular health than cholesterol alone.
The size matters because small, dense LDL particles (like "BBs") can easily lodge into and damage the delicate endothelial lining of your arteries, causing inflammation and plaque buildup. Large, fluffy LDL particles (like "cotton balls") are less harmful. Two people can have the same total LDL number, but the one with predominantly small, dense particles is at a much higher risk.
Systemic inflammation, measured by markers like CRP and Homocysteine, directly damages the endothelium—the thin, single-cell layer that lines all your blood vessels. This damage is a primary driver of cardiovascular disease. High inflammation makes the endothelial lining vulnerable to the buildup of plaque and the formation of blood clots.
Magnesium is crucial for heart health because it helps relax artery walls, which can lower blood pressure and reduce strain on the heart. It's involved in over 400 enzymatic reactions. A deficiency can contribute to arterial constriction and high blood pressure, increasing the risk of endothelial damage and heart disease.
This statistic highlights that cholesterol is not the whole story. You should be more concerned with the underlying factors that cause damage, specifically inflammation (CRP, Homocysteine), insulin resistance (A1c, Fasting Insulin), and the quality of your cholesterol particles (LDL particle number and size). Addressing these root causes is key to truly reducing risk.