Unlocking the Mystery of the Blood Brain Barrier and Its Impact on Brain Health
The Blood Brain Barrier: Your Brain's Protector
Understanding the Delicate Shield that Safeguards Your Brain
At the core of this discussion lies the blood-brain barrier – a critical component when exploring the connection between neurological disorders and brain health. This protective barrier is astonishingly thin, consisting of just a single layer of cells. In a similar vein to the concept of a leaky gut, the blood-brain barrier can also become compromised, giving rise to a condition known as a “leaky blood-brain barrier.”
Unveiling the Blood Brain Barrier
Peering into the Intricacies of Brain Protection
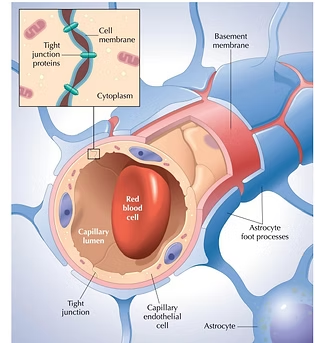
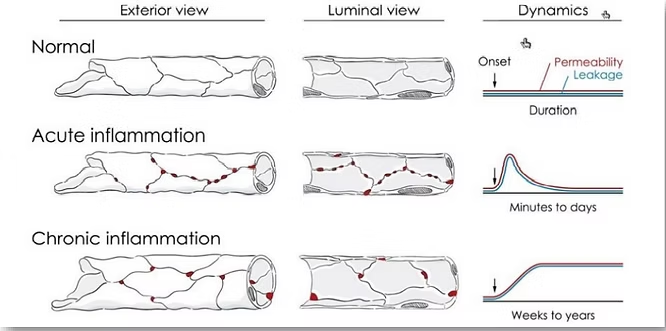
Imagine zooming in on a cross-section of your brain, focusing on the capillaries responsible for supplying blood to your brain’s cells. Here, you’ll find a layer of cells that acts as a partition between the bloodstream and the brain itself. This pivotal shield is what we refer to as the “blood-brain barrier.” Composed of numerous tight junctions, it serves to keep the brain sealed and secure. However, any disruptions in this barrier can lead to the brain “springing a leak,” resulting in a range of severe neurological problems.
Acute and Chronic Leaks: Unveiling the Consequences
Understanding Temporary and Long-lasting Breaches
Temporary breaches, caused by acute inflammation, can persist for a few minutes to days. On the other hand, chronic inflammation can result in leaks that last anywhere from weeks to years.
The Interplay Between Gut and Brain Health
It is worth noting that leaky gut and a leaky blood-brain barrier often go hand in hand. If you experience symptoms such as brain fog, brain fatigue, bloating, excess gas, or even constipation, it is possible that you may be grappling with both a leaky gut and a leaky blood-brain barrier.
Unveiling the Truth: Testing for Leak
Crucial Diagnostic Measures for Identifying a Leaking Blood Brain Barrier
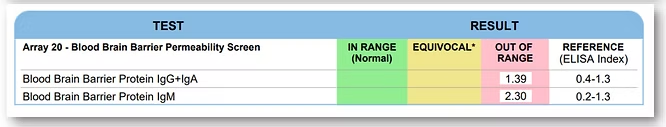
Thankfully, there are several tests available to determine if you are suffering from a compromised blood-brain barrier. One of the initial tests we conduct assesses blood-brain barrier permeability. The results are color-coded, with yellow or red indicating areas of concern. Examining sample patient reports reveals high protein levels associated with permeability, a clear sign of a leaky barrier.
Elevated levels from these tests may also indicate autoimmune diseases targeting the blood-brain barrier’s cells. Additional tests can specifically identify autoimmune diseases affecting various neurological tissues. The provided sample test results demonstrate five different tissue-related outcomes.
It is crucial to undergo testing if you experience these symptoms. Identifying a compromised blood-brain barrier early on allows you to take preventative measures against degenerative diseases like Alzheimer’s.
The Research: Illuminating the Connection
Insights into the Relationship between the Blood-Brain Barrier and Neurological Conditions
According to a recent review by Dr. Rajib Dutta, the disruption of the blood-brain barrier directly correlates with various neurodegenerative conditions. Among these conditions are Alzheimer’s, Parkinson’s, ALS, Huntington’s, Multiple Sclerosis, and more. This suggests that a leaking blood-brain barrier renders individuals more vulnerable to these diseases. Conversely, a healthy blood-brain barrier shields against such issues.
Dr. Dutta argues that a compromised barrier enables harmful blood components to seep into the central nervous system, making their clearance difficult, if not impossible.
Insulin: An Indication of Barrier Integrity
Exploring the Relationship Between Insulin and a Leaky Blood Brain Barrier
Insulin levels are optimally assessed while fasting, leading to the terminology “fasting insulin levels” in lab reports. The normal range for insulin typically falls between 2.6 and 24.9. However, the optimal level of fasting insulin is considered to be between 1 and 5. Unfortunately, one client’s levels exceeded 38, indicating high insulin levels and suggesting a predisposition to a leaky blood-brain barrier as well as Alzheimer’s.
Examining the Role of Homocysteine in Neurological Inflammation
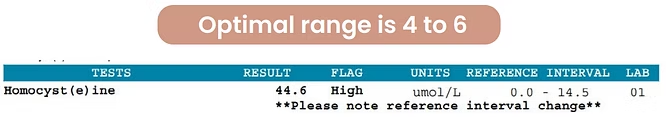
When reviewing lab results, the normal range for homocysteine levels usually spans from 0 to 14.5. However, it is essential to distinguish between “normal” and “optimal” levels. In this case, the optimal range for homocysteine in your system is actually 4 to 6. Shockingly, one of my clients displayed levels exceeding 44, indicating heightened levels of neurological inflammation.
The Impact on Parkinson's, ALS, and Multiple Sclerosis
Unveiling the Blood-Brain Barrier’s Role in Specific Neurological Disorders
Dr. Dutta’s paper illustrates the extensive research conducted worldwide to establish a connection between the quality of the blood-brain barrier and overall neurological health. The paper also explores how individual diseases are influenced.
Parkinson’s disease, for instance, can be initiated or exacerbated by the leakage of serum (the fluid in your bloodstream and its components) into the brain. This further promotes neurodegeneration within Parkinson’s patients.
ALS, an incredibly debilitating disease with a limited survival rate beyond five years, can experience motor neuron loss due to the degeneration of the tight junctions between cells, as previously mentioned. Markers assessing the condition of these junctions, as discussed earlier in this article, can be tested.
Multiple Sclerosis is closely tied to disruptions in the blood-brain barrier. If the barrier’s permeability is compromised, inflammation within the central nervous system can occur, often associated with metabolic dysregulation. For further information on this topic, I invite you to download my free resource: “Top 12 Must Know Inflammatory Lab Markers (and Their Optimal Ranges).”
Unveiling Additional Factors Influencing the Blood-Brain Barrier
It is important to acknowledge that traumatic brain injuries, particularly when they occur repeatedly, can disrupt the blood-brain barrier. This disruption can persist for years following the injury. In this context, the marker we can assess is called fibrinogen, which can indicate brain oxidative stress and potential damage. Fibrinogen testing must be conducted within 72 hours of the injury. Furthermore, epilepsy has also been associated with a dysfunctional blood-brain barrier.
Conclusion: Navigating the Path to Healing
Identifying Solutions to Repair and Protect the Blood Brain Barrier
A leaking blood-brain barrier can instill fear, given the severe long-term consequences it entails. Dr. Dutta emphasizes the importance of monitoring inflammation levels to identify the risk of these conditions and discover pathways for healing and safeguarding the blood-brain barrier.
Fortunately, various biomarkers can be assessed through simple blood work, offering a glimpse into potential healing solutions. Nutritional and lifestyle changes are often part of the equation. By analyzing your blood work results, we can evaluate factors such as gluten intolerance, vitamin D levels, fasting insulin levels, hormone imbalances, gut health, and much more to chart a personalized healing path.
Remember, your body possesses an innate healing ability that we can harness to restore your well-being.
Please don’t hesitate to reach out to me for consultations or appointments, which can be conducted virtually as well.
Frequently Asked Questions (FAQ)
The blood-brain barrier is a protective layer of cells that acts as a shield between your bloodstream and your brain. A "leaky brain" occurs when this barrier becomes compromised, similar to a "leaky gut." This allows harmful substances from the blood to leak into the brain, which can lead to inflammation and severe neurological problems.
Symptoms often include brain fog, brain fatigue, and other neurological issues. Because gut and brain health are closely linked, it frequently occurs alongside a leaky gut, which can cause symptoms like bloating, excess gas, and constipation.
Specific tests can assess blood-brain barrier permeability. These tests often measure antibody levels (like IgG, IgA, and IgM) associated with the barrier's cells. High levels indicate permeability or even autoimmune activity against the barrier. Other key blood markers include fasting insulin (optimal level 1-5 uIU/mL) and homocysteine (optimal level 4-6 umol/L), where high levels suggest inflammation and increased risk.
Research shows a direct correlation between a compromised BBB and neurodegenerative diseases. According to a comprehensive review, this includes Alzheimer’s disease, Parkinson’s disease, ALS, Huntington’s disease, and Multiple Sclerosis. A leaky barrier makes the brain more vulnerable to these conditions by allowing harmful blood components to enter the central nervous system.
Yes, identifying the problem is the first step toward healing. By analyzing biomarkers through blood work (such as inflammation markers, vitamin D, hormone levels, and gut health), a personalized healing path can be created. This often involves nutritional and lifestyle changes designed to reduce inflammation and support the body's innate ability to repair itself.