Part 4
Introduction to Neuroinflammation
Neuroinflammation is a complex process involving the activation of the brain’s immune response. It can lead to a variety of symptoms, including cognitive decline, mood disorders, and chronic pain. In this article, we will delve deeper into the science behind neuroinflammation, discuss its potential causes, and provide a comprehensive guide to treatment options.
The Science of Neuroinflammation
Neuroinflammation occurs when the immune system reacts to various stimuli within the brain. This reaction can lead to the production of inflammatory molecules, such as cytokines and chemokines, which can negatively impact the function of neurons and other brain cells.
Symptoms Associated with Neuroinflammation
Neuroinflammation can manifest in several ways, including:
1. Cognitive decline, such as difficulty with memory, concentration, and decision-making
2. Mood disorders, including depression, anxiety, and irritability
3. Chronic pain, particularly in the form of headaches or migraines
4. Sleep disturbances, including insomnia or excessive sleepiness
5. Fatigue or lack of energy
There are numerous factors that can contribute to neuroinflammation, including:
1. Infections, such as bacterial or viral infections that invade the brain
2. Autoimmune disorders, in which the immune system mistakenly attacks healthy brain tissue
3. Traumatic brain injuries, which can cause an inflammatory response in the brain
4. Environmental toxins, such as heavy metals or chemicals that can trigger inflammation
5. Genetic predisposition, where individuals may be more susceptible to neuroinflammation due to their genetic makeup
**The Functional Medicine Approach to Treating Neuroinflammation**
Diagnostic Testing for Neuroinflammation
A variety of tests may be ordered to help determine the underlying causes of neuroinflammation, including:
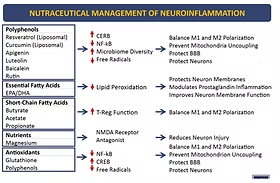
1. Vitamin D level: Low levels of vitamin D have been associated with increased inflammation in the body.
2. Food sensitivity testing: Certain food sensitivities can contribute to gut permeability, which may lead to neuroinflammation.
3. A1C and fasting insulin levels: These tests can help assess blood sugar control and insulin resistance, which can contribute to inflammation.
4. C-reactive protein (CRP) markers: CRP is a marker of inflammation in the body and can indicate the presence of neuroinflammation.
5. Hormone levels: Imbalances in hormones such as testosterone, estrogen, progesterone, and cortisol can contribute to neuroinflammation.
Personalized Treatment Plans for Neuroinflammation
Based on the results of diagnostic testing, a functional medicine practitioner may recommend a personalized treatment plan that may include:
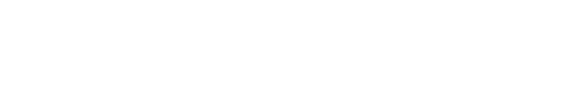
1. Dietary modifications: Eliminating food sensitivities and incorporating anti-inflammatory foods rich in polyphenols, essential fatty acids, and antioxidants.
2. Nutritional supplementation: Addressing deficiencies in vitamins and minerals that may contribute to inflammation, such as vitamin D, B vitamins, and magnesium.
3. Stress management techniques: Incorporating practices such as meditation, yoga, or deep breathing exercises to help reduce stress and its impact on inflammation.
4. Exercise: Engaging in regular physical activity to help reduce inflammation and promote overall brain health.
5. Sleep optimization: Ensuring adequate and high-quality sleep to support the body’s natural healing processes.
Functional neurology is an approach that focuses on strengthening the brain and improving its function through targeted neurological exercises. These exercises can help enhance neural connections, promote neuroplasticity, and ultimately reduce neuroinflammation. Some examples of functional neurology exercises include:
- Eye movement exercises: These exercises can help improve the function of the visual system and its connections with other areas of the brain.
- Balance and coordination exercises: By challenging the balance and coordination systems, these exercises can help strengthen the connections between the brain and the body.
- Cognitive exercises: Activities that challenge memory, attention, and problem-solving skills can help enhance overall cognitive function and reduce neuroinflammation.
The Importance of a Holistic Approach to Neuroinflammation
It is crucial to remember that neuroinflammation is a complex condition, and addressing it effectively often requires a multi-faceted approach. By combining functional medicine, personalized treatment plans, and functional neurology exercises, patients can experience significant improvements in their symptoms and overall brain health.
Conclusion: The Path to Better Health for Those Suffering from Neuroinflammation
Understanding the complexities of neuroinflammation and its impact on brain function is the first step towards finding relief from its debilitating symptoms. By partnering with a functional medicine practitioner and incorporating a holistic treatment plan, individuals suffering from neuroinflammation can embark on a path towards better health and improved quality of life.
If you or a loved one is experiencing symptoms of neuroinflammation, consider seeking the expertise of a functional medicine practitioner who specializes in this area. Through comprehensive diagnostic testing, personalized treatment plans, and the support of a knowledgeable healthcare professional, it is possible to reduce neuroinflammation and achieve better brain health.
Read more from the Neuroinflammation series:
Part 1 Brain on Fire
Part 2 Brain on Fire
Part 3 Brain on Fire
Part 4 Brain on Fire
Frequently Asked Questions (FAQ)
Neuroinflammation is the activation of the brain's immune response. It can lead to a variety of symptoms including cognitive decline (memory and concentration issues), mood disorders (depression, anxiety), chronic pain (especially headaches), sleep disturbances, and persistent fatigue.
According to the blog, potential causes include bacterial or viral infections that reach the brain, autoimmune disorders, traumatic brain injuries, exposure to environmental toxins (like heavy metals), and a genetic predisposition that makes some individuals more susceptible.
A functional medicine practitioner may use tests to uncover root causes, including: Vitamin D levels, food sensitivity testing, A1C and fasting insulin (for blood sugar control), C-reactive protein (CRP) as a general inflammation marker, and a full hormone panel to check for imbalances.
A holistic plan is multi-faceted and personalized. It can include dietary changes (removing food sensitivities, adding anti-inflammatory foods), targeted nutritional supplements, stress management techniques (meditation, yoga), regular exercise, sleep optimization, and functional neurology exercises to strengthen neural connections.
Functional neurology exercises are targeted activities designed to improve brain function. Examples include specific eye movements, balance and coordination drills, and cognitive challenges. These exercises aim to enhance neuroplasticity, strengthen neural pathways, and thereby help reduce neuroinflammation and improve symptoms.